FOCUSED ON THE DEVELOPMENT OF TRANSFORMATIVE THERAPIES FOR THE TREATMENT OF :
Worsening heart failure
Hyponatremic acute heart failure
Worsening heart failure
Worsening heart failure
Worsening heart failure
AVP
Biology
Elevated circulating vasopressin concentration has been reported in heart failure (HF) patients and in preclinical HF models. High vasopressin levels contribute to
- Deterioration of cardiac function through V1a receptor
- Systemic congestion and hyponatremia through V2 receptor
- Glucose metabolism impairment and increased sympathetic tone through its third receptor V1b.
In autosomal dominant polycystic kidney disease (ADPKD), vasopressin has been found to be involved in the pathogenesis of the disease
- The cysts in polycystic kidney disease (PKD) derive predominantly from vasopressin sensitive tubular segments expressing V2 receptors, i.e. the collecting duct and the distal nephron.
- AVP has been shown to directly regulate cyst growth in the kidney with abnormal excessive fluid secretion, as well as excessive proliferation and apoptosis of the tubular epithelial cells
Strategy
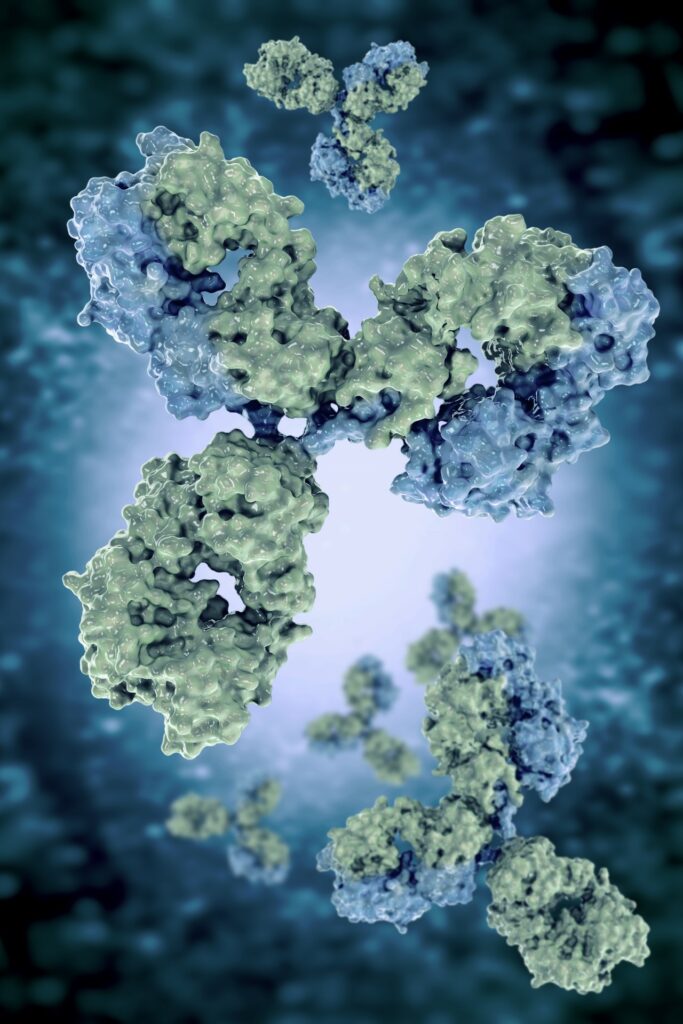
In order to inhibit the full spectrum of vasopressin activity, its 3 receptors (V1a, V1b and V2) should be equally blocked to avoid the overstimulation of an unblocked receptor subtype. This has not been achieved with small molecule receptor antagonist approach. The alternative strategy we are pursuing is to selectively neutralize vasopressin with a human monoclonal antibody that will suppress activation of the 3 receptor subtypes. The expected rapid benefit would be
- the restoration of normal natremia in AHF patients with the reduction of intravascular and tissue congestion.
- The modification of the disease course in ADPKD.